Prostatitis is one of the main urological problems in men under 50 years of age. Ten to twelve percent of all representatives of the stronger sex have experienced symptoms of prostatitis at least once in their lives. The disease can occur in an acute or chronic form, on which its signs and symptoms directly depend.
What is prostatitis
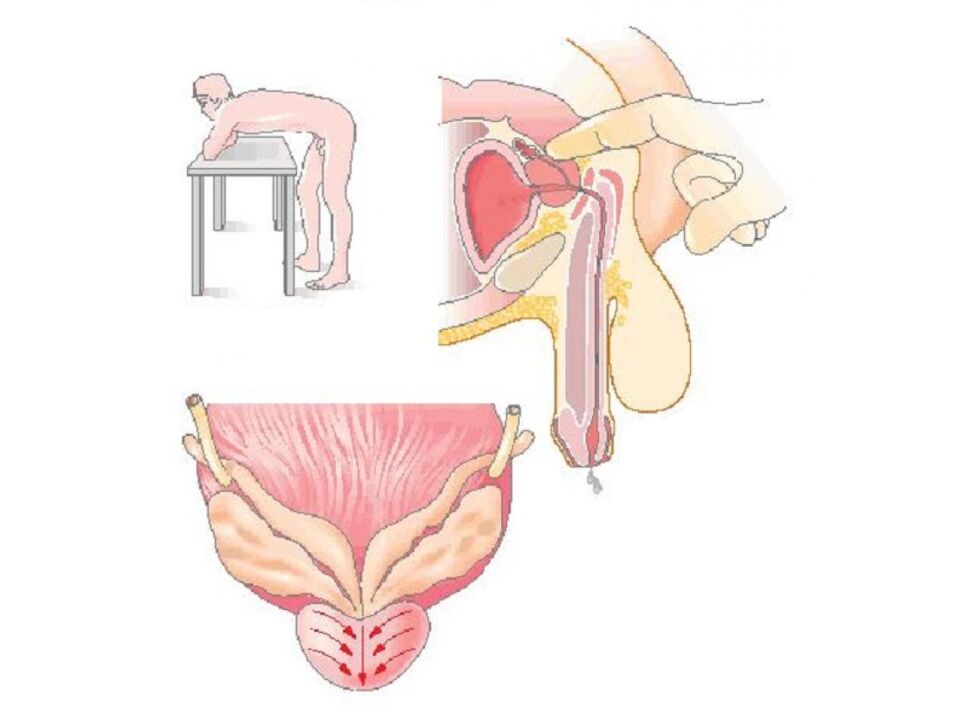
Prostatitis is a term that means inflammation of the prostate gland.The prostate or prostate gland is an organ of the male reproductive system. Its normal size does not exceed the size of a walnut. The gland is located under the bladder, in front of the rectum. The prostate surrounds the urethra, the tube through which urine and sperm leave the body. Its main function is the production of secretions (prostatic juice), which supports the vital activity of sperm after ejaculation.
The inflammatory process in the prostate can be caused by an infection, but also by various other reasons.
Types and first signs of the disease
The first signs and further symptoms will depend on the type of prostatitis. In total, clinicians distinguish 4 types.
- Acute bacterial prostatitis: Caused by a bacterial infection, it usually has a sudden onset that may resemble flu-like symptoms. This is the rarest of the four types of prostatitis.
- Chronic bacterial prostatitis: Characterized by recurrent bacterial infections of the prostate. There may be few or no symptoms between attacks, which is why it can be difficult to treat successfully.
- Chronic prostatitis/chronic pelvic pain syndrome: Most cases of prostatitis fall into this category, but at the same time this type is the least understood. It can be characterized as inflammatory or non-inflammatory, depending on the presence or absence of infection-fighting cells - antibodies in urine, semen and prostate secretions. It is often impossible to determine one specific cause. Symptoms may come and go or remain intermittent.
- Asymptomatic inflammatory prostatitis: This disease is often diagnosed incidentally during treatment for infertility or prostate cancer. People with this form of prostatitis do not complain of symptoms or discomfort, however, tests show the presence of infectious cells in the secretions of the prostate.
Main symptoms
Symptoms associated with prostatitis can vary depending on the underlying cause of the disease.Common symptoms that gradually increase include:
- pain or burning when urinating (dysuria);
- difficulty urinating, such as a thin stream of urine or sluggish, intermittent urine;
- frequent urination, especially at night (nocturia - going to the toilet more than 2 times during the night);
- urgent urge to urinate.
An important symptom is pain, which may occur or radiate to different parts of the lower body. she can be:
- in the rectum (rectal), sometimes in combination with constipation;
- in the abdomen and/or lower back;
- in the perineum - between the scrotum and rectum.
Patients often report discomfort in the penis and testicles. Painful ejaculation is characteristic, and in addition, prostatitis can be accompanied by a sexual disorder.
A rapid and severe onset is usually characteristic of the acute bacterial form, which is characterized by an additional complex of symptoms similar to that which occurs during the influenza virus.This:
- fever and chills;
- general weakness and body aches;
- enlarged lymph nodes;
- dry throat.
If the patient ignores the first signs of the disease and does not seek help from a urologist-andrologist, then there are dangerous cases of purulent complications. Acute infectious prostatitis can develop into a severe form of pathology, when the prostate tissue becomes covered with pustules or abscesses. Symptoms include the following:
- cloudy urine or blood in the urine;
- discharge from the urethra;
- bad smelling urine and discharge.
If he discovers the initial signs of inflammation, a man should immediately consult a doctor for further diagnosis.
Diagnostic methods
Prostatitis is usually diagnosed by laboratory testing of a urine sample and examination of the prostate by a urologist.This exam involves palpating the prostate through the rectum to check for any abnormalities. Sometimes the doctor collects and tests a sample of prostate secretions. To obtain it, the urologist massages the gland during a rectal examination. Because there is concern that the procedure could release bacteria into the bloodstream, this test is contraindicated in cases of acute bacterial prostatitis.
The urologist also takes body temperature in the armpit and rectally, and then compares the results. During acute prostatitis, the temperature in the anus will vary upwards by about 0. 5 degrees.
Laboratory tests
Laboratory tests that may be ordered include:
- clinical analysis of blood and urine;
- bacterioscopy and culture of urine sediment and prostate secretions - examination of samples under a microscope for the presence of bacteria;
- smear of discharge from the urethra (if there is discharge);
- determination of prostate specific antigen (PSA) level.
If a clinical blood test shows an elevated level of leukocytes (from 10-12 per visual field), this will indicate the presence of inflammation. Acute infectious prostatitis is characterized by an increase in neutrophils, a type of white blood cell whose main function is to destroy pathogenic bacteria. There is also a decrease in the level of eosinophils (below 1% of all leukocytes), another group of leukocytes responsible for protecting the body from proteins of foreign origin. The reaction of sedimentation of erythrocytes or red blood cells is another indicator of a general clinical blood test and also indicates the presence of a pathological process in the body if its value exceeds 10 mm/h. The rate of sedimentation of these blood cells increases with the increase in the concentration in the blood plasma of markers of the inflammatory process: protein fibrinogen and immunoglobulin, as well as C-reactive protein.
Bacterioscopy of urine sediment and prostate secretions will indicate the presence and number of pathological microorganisms in these biological fluids, and thanks to the antibiotic sensitivity culture, the type of bacteria will be determined for further treatment selection. The causative microorganism can be determined, among other things, by taking a smear from the urethra for microscopic examination.
The prostate specific antigen test is a screening test in the form of an intravenous blood test for a protein produced exclusively by prostate cells. The protein norm depends on a man's age and ranges from 2. 5 ng/ml for men aged 41-50 to 6. 5 ng/ml for men over 70 years old. An increase in the level of this protein above the age norm means the need for a biopsy - tissue analysis for oncology. However, excess protein can also be seen due to inflammation of the prostate.
PSA levels may also rise slightly with benign enlargement (adenoma) of the prostate and as a result of urinary tract infections.
PSA age norms - table
| Age category | PSA norm |
|---|---|
| Under 40 years old | less than 2. 5 ng/ml |
| 40–49 years old | 2. 5 ng/ml |
| 50–59 years old | 3. 5 ng/ml |
| 60–69 years | 4. 5 ng/ml |
| Over 70 years | 6. 5 ng/ml |
Instrumental studies
Since none of the tests or analyzes individually provide a complete guarantee for the correct diagnosis, other methods - instrumental - can be used as part of a comprehensive diagnosis. This includes:
- Urodynamic study of the urinary bladder- a complex instrumental method using special equipment allows you to determine whether the bladder is completely emptied, the rate of urine flow, pressure inside the bladder and urethra, as well as to assess the effect of prostatitis on normal urination. This study is recommended for people with chronic problems of the urinary system: occasional or thin stream, incontinence, frequent urination, etc. It is also indicated for patients with prolonged inflammation of the prostate, especially when standard therapy is ineffective. Before the examination, a special catheter-sensor is introduced into the patient's urethra in a horizontal position, which is also connected to the measuring equipment. Then he is asked to drink a certain amount of clean water, simultaneously recording the feeling of a full bladder, the first urge to urinate, the presence of leakage of urine, etc. Then the patient is transferred to a specially equipped chair, on which he will have to relieve himself while still under the control of sensors and equipment that performs the necessary measurements. The procedure consists of several stages, each of which takes about half an hour. The results of the urodynamic study are given to the patient immediately after its completion.
- Ultrasound Imaging (USA)- the method is used for the diagnosis of existing disorders, and it is also indicated for men after 45 years of age as a prevention of prostatitis and other glandular diseases. The study is performed in the morning on an empty stomach with an ultrasound machine through the front abdominal wall with a bladder filled with clean water, as well as by inserting a special sensor 5-7 cm deep into the rectum (rectal method) or through the urethra. The procedure is absolutely safe and allows you to determine the contour, size and condition of certain areas of the prostate. The volume of a healthy prostate is approximately 20-25 cm3. The maximum length, width and thickness are 3. 5 cm, 4 cm and 2 cm.
- magnetic resonance imaging (MRI)- the method allows you to study in detail the structure, density, condition and even blood flow of the prostate; sometimes, for a better examination, an additional contrast agent is injected intravenously. The examination is also carried out to distinguish prostatitis from oncology. The MRI machine is a large cylinder surrounded by a magnet, into which, like a tunnel, the medical table with the patient slides. The person should wear loose clothing without metal fittings and refrain from heavy food 10-12 hours before the procedure. Before the examination, it is mandatory to remove watches, jewelry and all other metal objects. If the patient has implants or heart devices that contain metal in the patient's body, the diagnostic method MRI is contraindicated. To perform the procedure, a transrectal sensor is most often used (although it is possible without it), having previously cleaned the rectum with an enema. The nurse inserts the sensor and secures it with a special disposable cuff. During the entire duration of the examination, which is about 30 minutes, the patient should lie as still as possible. The procedure is painless.
- Cystoscopy- examination of the mucous membrane of the urethra and bladder using a cystoscope - a long, narrow catheter with a bulb and a camera at the end under local anesthesia. The procedure is performed after the bladder is full. The duration of cystoscopy is about 15 minutes. The method allows you to assess the condition of the urinary tract, excluding other possible diseases that cause problems with urination.
- Prostate biopsy- is a necessary procedure if, after a comprehensive examination, the doctor suspects a malignant process in the prostate. It must be turned off or confirmed to select a treatment tactic. The procedure is performed on an outpatient basis by inserting a puncture needle through the patient's rectum and taking a sample of prostate tissue. A local anesthetic is injected into the anus, and then, when it has begun to work, an ultrasound probe with a needle attachment is inserted into the intestine. Under the supervision of ultrasound, the surgeon determines the places from which it is necessary to "pinch off" the material for analysis. There are usually up to 18 different points on the organ. The biopsy does not cause pain, after the anesthesia wears off, only slight discomfort is possible.

%20and%20inflamed%20(right)%20prostate%20on%20MRI%20scans.jpg)
If the patient experiences recurrent episodes of urinary tract infection and prostatitis, the specialist will prescribe a complete comprehensive examination of the genitourinary system to identify anatomical abnormalities.
Differential diagnosis
Symptoms of acute prostatitis may resemble inflammation of the bladder or urethra. In all cases, symptoms include painful and frequent urination. But acute prostatitis is characterized by vivid symptoms of general intoxication and admixture of pus in urine and secretions. Palpation of the prostate will be painful and will reveal an increase in the size of the gland, which will not happen with cystitis or urethritis.
Doctors say that inflammation of the prostate does not increase the risk of prostate cancer.
Chronic prostatitis should be differentiated in young men with anogenital symptom complex and vegetative urogenital syndrome. These diseases can only be distinguished by analyzing prostate secretions for the presence of bacteria. In men over 45 years of age, it is necessary to rule out oncology and prostate adenoma, which are usually asymptomatic in the initial stages, unlike prostate inflammation. For a more detailed analysis, the urologist will prescribe a PSA test and then, if necessary, a biopsy.
Prostatitis can be an acute bacterial disease, which is often easily treated with antibiotics, or a chronic disease that recurs and requires constant medical supervision and control. In any case, only a specialist in the field of urology and andrology can correctly diagnose the disease.





























